How Pathos AI is Revolutionizing Cancer Treatment for Patients
Cancer drug development has long been hindered by high failure rates, long timelines, and soaring costs. Traditional approaches often rely on trial-and-error methods, with over 90% of oncology drugs failing in clinical trials—many due to poor target selection or an incomplete understanding of tumor biology. The process can take over a decade and cost billions, while treatments are typically designed for broad populations, limiting their effectiveness for individual patients.
Not to mention that critical data such as genomic, clinical, and imaging information—has historically been fragmented, making it difficult to generate the insights needed for more precise therapies.
Where others see obstacles, Pathos AI sees an opportunity to reinvent. Rather than offering incremental improvements, Pathos is re-engineering the entire drug development process which placing precision medicine at its core and transforming how we fight cancer.
Before understanding the heart of their technology, let’s start with the beginning of Pathos AI.
Pathos AI – From Personal Pain to Savior
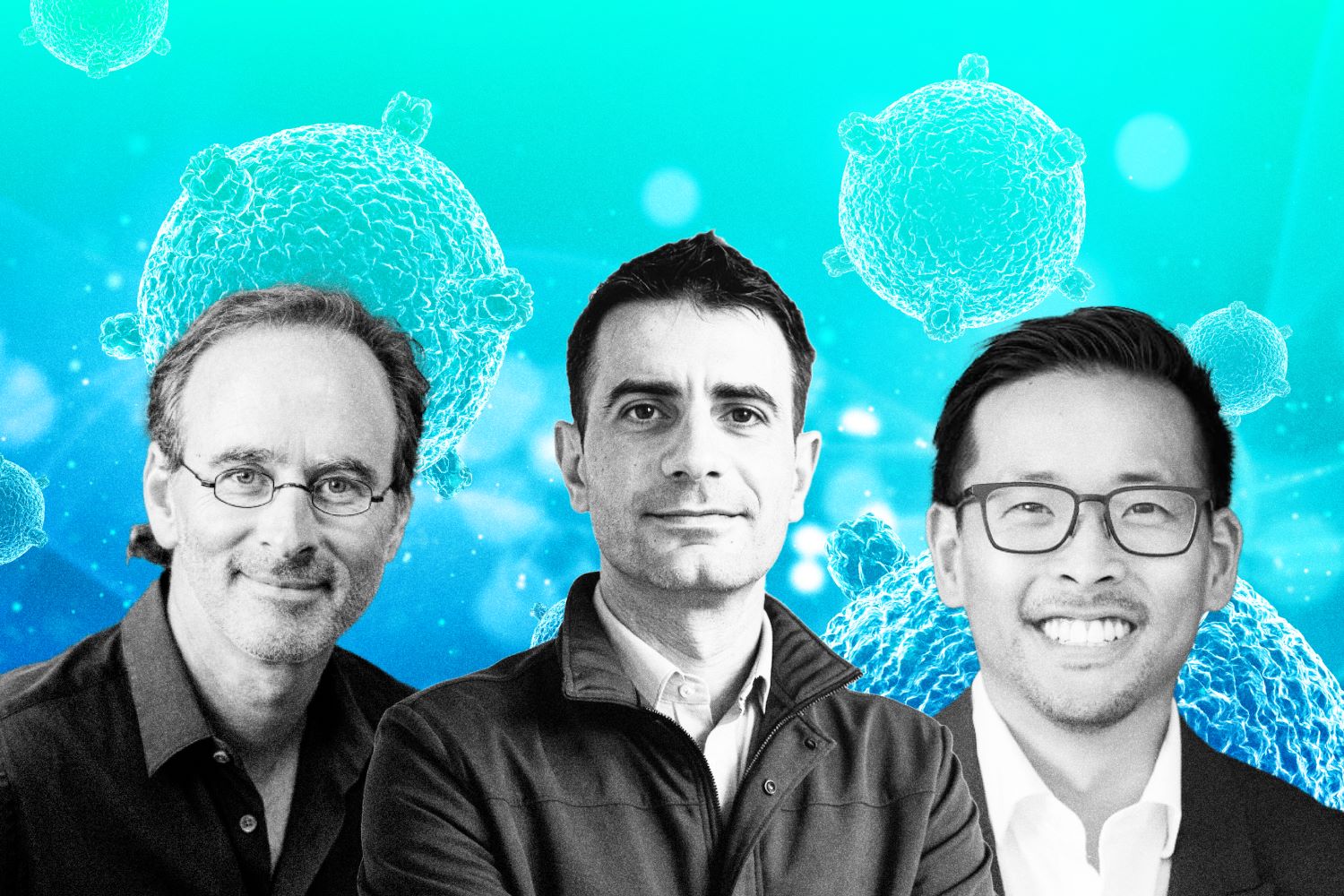
When we talk about Pathos AI, we need to bring Ryan Fukushima to the table. A seasoned entrepreneur at the intersection of AI and precision medicine, Fukushima co-founded Pathos in 2022 alongside Eric Lefkofsky, building on years of experience from his time helping launch and scale Tempus AI.
At Tempus, Fukushima witnessed firsthand how fragmented data and outdated systems were holding back progress in personalized medicine. That experience shaped his conviction: AI could not only help doctors make better decisions but also revolutionize how drugs are discovered and developed.
That was only part of the reason Pathos AI came to life. Ryan Fukushima didn’t just witness the pain points of oncology drug development—he lived through the personal pain of losing a loved one to cancer.
“There’s no worse feeling than watching a loved one fight bravely through a cancer diagnosis and battle through treatments while hoping for a miracle or a little more time. Suddenly, your doctor tells you that there’s nothing more they can do, and that palliative care is the only option left. The crushing feeling of hopelessness sets in, and it’s a moment that sits with you forever,” Ryan shared in his article on Medium.
He added, “Sadly, this is an experience shared by far too many families around the world. I know this all too well because I was there with my own family. It’s a moment etched in my memory, a moment that has fueled my desire to make a difference.”
That’s how Pathos AI came to life—born from both professional insight and personal conviction. Now, let’s take a closer look at the core technology that powers their mission to transform cancer care.
An Integrated Suite Powering the Future of Cancer Therapeutics
Pathos AI has built a powerful set of tools to make cancer drug development faster and smarter. At the center is the PathOS™ platform, which uses advanced AI to help discover and develop new, targeted cancer treatments. Backed by their own AI technology and a growing pipeline of drug candidates, Pathos is working to turn scientific discoveries into real medicines more efficiently. Here’s a closer look at what they offer.
PathOS Platform
PathOS™ is Pathos AI’s powerful platform built to speed up and improve how cancer drugs are discovered and developed. It brings together advanced AI technology and lab testing to help find the right treatments for the right patients more quickly. The platform is designed to deliver insights at every stage—from early research to real-world use.
PathOS uses some of the largest and most detailed cancer datasets available. With this information, its AI system constantly learns and updates itself, predicting which groups of patients are most likely to benefit from a specific drug. This helps researchers focus on the most promising treatment options and design better-targeted therapies.

To test these predictions, Pathos runs lab experiments using real patient samples and organoids—small tumor models grown in the lab. By studying how cancer cells respond to different drugs, the team can confirm if a treatment is likely to work for certain patients. This makes clinical trials faster, more accurate, and more likely to succeed.
The platform also includes a smart engine that can automatically find and rank new drug targets. It connects all the data from the lab, clinical trials, and real-world patient results to build models that guide drug development from start to finish.
Because it’s built on a modern data system, PathOS gets smarter with every new piece of information. It brings together data from every step of the process, making sure nothing is missed. This helps Pathos move quickly and confidently from early drug discovery to real treatments for patients.
Powerful Pipeline
One of their main drugs is pocenbrodib. It works by blocking proteins (CBP/p300) that help cancer cells grow—especially in prostate cancer. This drug is being tested in patients with advanced prostate cancer, both on its own and combined with other treatments. It may also help in other cancers like multiple myeloma and breast cancer.
Another important drug is P-500, which targets an enzyme called PRMT5. This enzyme helps cancer cells survive and spread. P-500 is special because it can reach the brain, making it useful for hard-to-treat cancers like high-grade glioma and uveal melanoma. Early tests show it works well and might also boost the effects of other treatments when used together.
Pathos AI uses a powerful platform called PathOS™ to guide all this work. It helps them find the best drug targets, predict which patients will benefit most, and design better clinical trials—all using real patient data and AI.
Major Funding Milestones that Fuels Pathos AI’s Growth
In July 2021, Pathos AI secured its Series A funding round, raising $10 million. This early-stage capital was instrumental in building the company’s foundational AI platform, which integrates multi-omic data to identify novel cancer therapies. The funding allowed Pathos to expand its research team and begin validating its approach in preclinical settings.
By March 2023, the company had made significant progress, leading to a $30 million Series B round. This round supported the initiation of Phase 1 clinical trials, marking a major milestone as Pathos transitioned from discovery to early-stage human testing. The funding also helped scale its AI infrastructure and deepen its partnerships with academic and clinical institutions.
In October 2024, Pathos AI raised $62 million in Series C funding. This round was led by New Enterprise Associates and aimed at advancing the company’s Phase 2 clinical programs. The capital was also used to enhance its proprietary AI models, which are designed to predict patient responses and optimize trial design.
The most transformative moment came in May 2025, when Pathos closed a $365 million Series D round, bringing its valuation to $1.6 billion. This round was driven by growing confidence in the company’s platform and its potential to reshape oncology drug development. The funding is being used to develop a foundation model for cancer biology, in collaboration with AstraZeneca and Tempus, and to expand its clinical pipeline across multiple tumor types.
“With this financing, we’re building one of the most advanced AI engines, designed to accelerate development, deepen clinical insight, and ensure the right therapies reach the patients who need them most,” Pathos AI CEO Iker Huerga said.
The Ongoing Risks and Challenges
Pathos AI’s future hinges heavily on the success of its clinical programs, particularly the upcoming Phase II trials for its lead candidates, P-300 and P-500. These trials are designed to validate the efficacy and safety of its AI-predicted therapies in larger, more diverse patient populations.
If the real-world outcomes diverge from the platform’s predictions, it could cast doubt on the reliability of its models. Such a scenario would not only delay regulatory approvals but could also erode investor confidence and stall momentum in both product development and strategic partnerships.
Another significant challenge lies in the regulatory landscape, which is still catching up with the rapid integration of AI in drug development. Regulatory bodies like the FDA and EMA are actively working to define frameworks for evaluating AI-driven platforms. Pathos must ensure its models are transparent, explainable, and validated across diverse datasets.
Moreover, it must comply with stringent data privacy regulations such as HIPAA and GDPR, especially given its reliance on sensitive multi-omic and clinical data. Any misalignment with these evolving standards could result in trial delays, additional compliance burdens, or even legal challenges.
Is AI Making Doctors Obsolete?
According to Ryan Fukushima, the future of healthcare isn’t about replacing doctors with AI—it’s about empowering them. As someone who works at the intersection of healthcare and artificial intelligence, Fukushima believes AI’s greatest potential lies in freeing up professionals to focus on what they do best: strategic thinking, clinical judgment, and patient care.

He explains that AI can handle 60 to 80 percent of the repetitive, monotonous work that slows down drug development and clinical practice—things like paperwork, data entry, or basic analysis. These tasks are essential, but they aren’t where human expertise is most valuable. By automating them, AI unlocks time and energy for professionals to focus on the complex decisions that truly impact outcomes.
But Fukushima is clear: AI is not meant to make decisions for doctors—it’s meant to organize the overwhelming flood of medical data in a way that helps doctors make smarter, faster, and more personalized decisions with their patients. In other words, AI becomes the assistant, not the authority. He emphasizes that trade-offs in medicine are rarely black and white, and those nuanced, human-centered choices will always require a doctor’s judgment.
He compares the shift to what happened in aviation. “Planes can take off and land automatically today,” he says, “but no one wants to fly without a pilot.” Just like autopilot didn’t eliminate pilots, AI won’t eliminate physicians—but it will change their role. Doctors who adopt AI will have the equivalent of a thousand digital assistants, while those who resist it risk falling behind.
In Fukushima’s view, the doctors and drug developers who learn how to harness AI won’t just survive—they’ll become the 10x version of their peers. “It’s not AI vs. doctors,” he says. “It’s doctors with AI vs. doctors without it.” And that difference, he believes, will define the next generation of healthcare leadership.