How Trinity Health “Strikes Gold” with Wise Strategies to Elevate Patient Engagement
Based in Livonia, Michigan, Trinity Health is now one of the largest multi-institutional Catholic healthcare delivery systems in the U.S, serving diverse communities that include more than 30 million people across 25 states. Committed to those who are poor and underserved in its communities, Trinity Health is known for its focus on the country’s aging population.
While active patient engagement in healthcare has been proved to lead to better health outcomes and lower costs, research shows us that the majority of patients today find it’s not easy to obtain information about their conditions and services due to the complexity of modern healthcare systems. In practice, most health care delivery falls far short of achieving that effective patient engagement.
Many private and public healthcare organizations are now seeking strategies to better educate their patients and making them part of the decision-making process. We can see that patient engagement is increasingly recognized as an integral part of healthcare and a critical component of safe people-centered services, not except Trinity Health.
Patient Engagement Is an Ultimate Priority
“Trinity Health’s ongoing work to improve patient engagement and the patient experience across its states is supported and driven by our leaders’ commitment to the effort. With support from executive leadership, we are establishing Patient and Family Advisory Councils at all of our member hospitals as a means to amplifying the voice of our patients,” said Prabhjyot Singh, Director of People-Centered Care Experience at Trinity Health.
Besides patient engagement, there’s a need to engage with their member health systems. Trinity identified engagement as a key aspect of the organization’s system-wide effort to deliver high-quality health care and described the role of the corporate leadership. An important consideration is balancing consistency in the approach across member hospitals.
The report “Organizational-Level Consumer Engagement: What It Takes” from the Center for Consumer Engagement in Health Innovation and the Health Care Transformation Task Force comprehensively details the efforts at Trinity that have made commitments to implementing consumer engagement strategies.
According to the document, Trinity uses a wide range of strategies to engage with their local hospitals and identify opportunities for improvement at the organization-wide and local levels, including developing common resources, connecting leaders, setting goals for the implementation, holding regular meetings, and convening health system leaders, which were categorized into two broader buckets.
#1: Standardizing and Spreading Best Practices
Patient and Family Advisory Council Implementation
The Patient and Family Advisory Councils (PFAC) strategy is the most comprehensive engagement strategy implemented by members of Trinity. As each local entity establishes its PFAC, the primary role of Trinity’s corporate leadership is to set goals for PFAC adoption and provide support to individual hospitals by providing standardized tools and creating cross-organization connections to support shared learning.
In recognition of the need for flexibility at the local level, the specific approach to implementing the PFACs is ultimately determined by each local member health system. Trinity also acts as a convener to help connect member hospitals that are early on in PFAC implementation or experiencing specific challenges with operating their PFACs to hospitals with more mature PFACs to aid in the sharing of best practices.
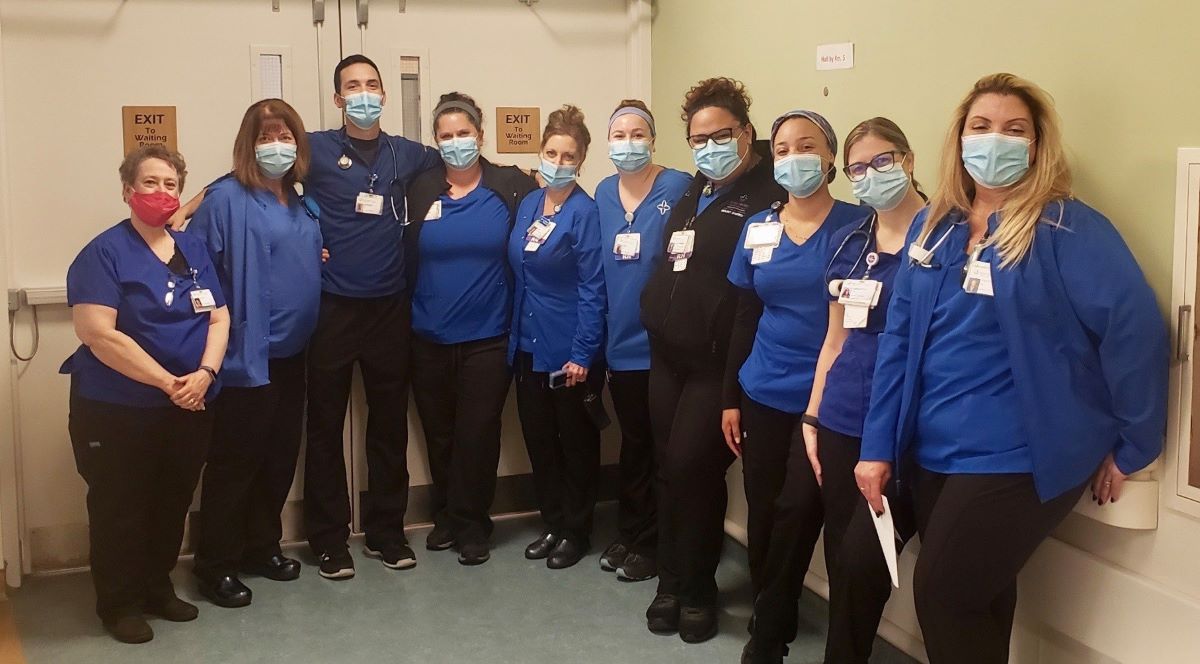
This is accomplished using Regional Patient Experience Teams in some Trinity regions. These teams are comprised of patient experience leaders and the chief nursing officer from multiple entities in a given region. These teams meet monthly to discuss local or regional progress on the establishment and operation of PFACs and to develop work plans for improving patient experience.
The Importance of Nurse Leader Rounding
Trinity emphasized the importance of nurse leader rounding as a system-wide strategy for engaging with people during inpatient visits and proactively working to identify opportunities to improve care. Trinity Health has set goals for the implementation of nurse leader rounding programs throughout its network of health systems. In nurse leader rounding, a nurse leader visits a patient to discuss the quality of care they have received and gather feedback on their overall experience.
The nurse leader asks the patient for feedback on staff communication, responsiveness, experience with hourly rounding, pain control, and other feedback that would improve their stay. There is no specific feedback mechanism to communicate the impacts or results of the rounding back to patients. Rather, the focus of this effort is to engage patients on an ongoing basis to identify and address potential issues in real-time.
Ideally, every patient with an inpatient will experience a nurse leader rounding session every day. Many of Trinity’s hospitals have adopted “protected time” for nurse leaders to complete rounding. At some hospitals, the results of rounding sessions are recorded in an electronic format and aggregated for review at the hospital unit during regular meetings, and they may be reviewed by others all the way up to the corporate leadership.

#2: Informing System-wide Operations
Focus Groups with Focused Feedbacks
Trinity uses focus groups to engage people and gather targeted feedback to provide input on specific topics. Generally, focus group participants are recruited from local PFACs with a focus on identifying people who have an interest in or patient experience with the specific topic areas being covered in each focus group. Focus group feedback is aggregated and communicated to the Trinity staff leading the specific project area on an ongoing basis.
People-Centered Care Experience Cabinet
At Trinity, the People-Centered Care Experience Cabinet (PCCEC) is a monthly meeting comprised of hospital-level patient experience leaders from various regions. At these meetings cabinet, members discuss the potential impacts of changes on patient experience and develop strategies to improve and promote consistency across Trinity’s health systems network.
Integrated Clinical Leadership Meetings
Trinity leaders hold monthly meetings with leadership teams to review performance against initial strategies and goals. Meetings include clinical leaders such as the chief, medical officer, chief nursing officer, pharmacy director, accountable care organization leaders at each hospital, together with Trinity’s executives. Seeing PFACs at the local level as a focus, these meetings review the status of each PFAC rollouts to identify potential resource requirements and opportunities.
Trinity Health at Home: A Move to Remote Engagement with RPM
By the time of 2020, Trinity started to realize that keeping patients out of the hospital and the emergency department (ED) by helping them stay healthier at home is critical. To achieve that, they came up with the idea of the Trinity Health At Home program using remote patient management (RPM). They knew RPM technology could help, but they also understood that technology alone wasn’t the solution.
The average age of the patients who became part of the Trinity Health At Home program is 75. Those patients didn’t grow up using our modern technology, so Trinity needed to find a high-technology program that could effectively monitor the health status of high-risk patients at their homes. That program needed to be easy to understand and use. Among many programs on the market, Trinity chose to partner with Vivify.
From the beginning, Trinity had very clear goals for its Trinity Health At Home program. One was to reduce preventable hospital readmissions, as entering the hospital, or even going to the ED, is tremendously disruptive to the lives of patients. If they could head off events that lead to hospital readmissions and ED visits, it would improve the quality of life for the patients and their families.
Also, Trinity wanted to reduce the number of Pro Re Nata (PRN) visits, which mean “as needed” or “when necessary” visits to the home by nurses. PRN visits are relatively expensive and time-consuming. In an era where there are already nursing shortages in many areas, the total time required for an in-home visit to address issues that could have been avoided by RPM technology is the time taken away from helping other patients.

According to the PRN provider Vivify, the important point here is that no matter how brilliantly designed a program is, no matter how sophisticated the technology behind it is, no matter how much money the executive team or C-suite puts behind it, the simple fact is an RPM program won’t work if it isn’t being used. Trinity understood this principle and went to great lengths to ensure both providers and patients understood the potential benefits and became fully engaged in it.
Bringing Physicians and Nurses On-Board
To clinicians, the ultimate motivator in the adoption of new technologies is how it will help improve their ability to drive better health outcomes for their patients. They seemed to be frustrated by new technologies and workflow changes that create extra work without delivering additional value. Trinity knew this, and so it worked with Vivify to educate clinicians on how the RPM program could help them become more efficient while helping patients achieve their health goals while staying at home.
Trinity also understood that having willing participants among the staff was key to success. As their roles would be changing, Trinity had all staff members re-interview for their jobs to be sure they would have the right people in place to launch the program. Once staffing was set, they were shown how to use the technology to monitor patients and what the process should be if something was going wrong.
Physicians were also shown how technology could help them unclog overloaded waiting rooms and reduce their workloads while increasing patient satisfaction. Fewer office visits meant more time to work with those patients who needed more attention, and more time to get to know the stories behind the patients in order to drive better outcomes.
Ensuring Compliance from Patients and Caregivers
Compliance represented one of the greatest challenges. Trinity Health At Home begins generating enthusiasm among patients and caregivers while the patient is still in the hospital. The home care coordinator explains that the patient’s doctor thought that the patient should participate in the program and shows a video that explains the Trinity Health At Home program and how it works and then how to use the tablet.
The home care coordinator then demonstrates how easy it is to take readings using the supplied equipment and to use the tablet to answer simple questions such as how the patient is feeling that day. Once the patient is intrigued, the home care coordinator asks for consent to participate in the Trinity Health At Home RPM program. By that point, very few patients decline to give it a try.
Then when the patient goes home, Trinity Health At Home schedules a nurse visit to not only help the patient get settled in, but also to bring and set up all the RPM equipment, make the wi-fi and Bluetooth connections, and show the patient and caregiver how to use the equipment and report results in more detail. The nurse can answer any additional questions and ensure that the patient has everything needed for the program to operate smoothly.
It’s important for the RPM program to be presented in a way that makes patients feel that the nurses they work with are part of Trinity rather than outside contractors. This helps strengthen the relationship between the patients and Trinity’s staff and reinforces the idea that it is a total healthcare solution. As a result, Trinity Health At Home reached a 90% compliance rate all the way through the program, which was very astounding.
The Bottom Lines
As greater engagement in healthcare leads to improved outcomes, Trinity Health has done a good job of implementing various strategies at different levels, in order to engage not only with the patients but also with the staff and leadership teams throughout its network of healthcare systems and local hospitals. I believe those strategies have left many important lessons for today’s healthpreneurs.